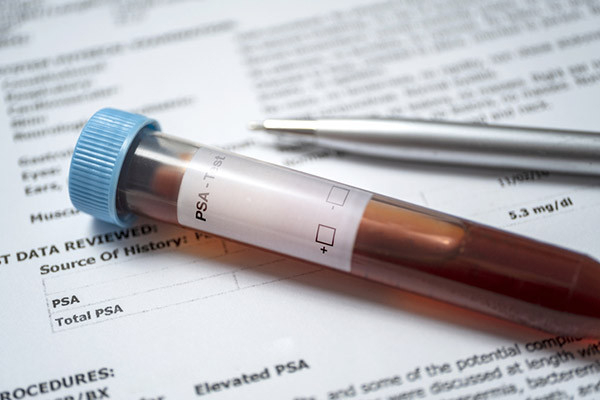
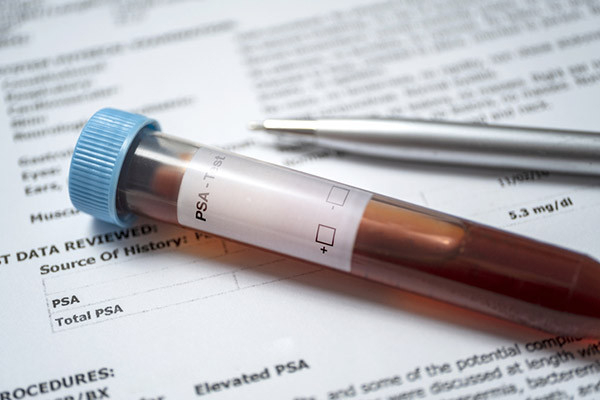
Screening tests, such as Pap smears or blood pressure checks, could save your life. They can detect a disease you have no reason to suspect is there. Early detection may allow treatment while a health condition is curable and before irreversible complications arise.
Some screening tests help prevent the disease they are designed to detect. For example, colonoscopies and Pap smears can identify precancerous abnormalities that can be addressed so they cannot continue to grow and become cancerous. And missed screening tests contribute to thousands of avoidable deaths each year in the US. Yet there’s a point of diminishing returns, as a new study on Pap smears illustrates. And many of us could benefit from a better understanding of the limits of screening, and how experts decide when people should stop routine screening tests.
Know the limits of screening tests
Even the best screening test has limitations. It can miss the disease it’s intended to detect (false-negative results). Or it can return abnormal results when no disease is present (false-positive results).
Equally important, as people grow older life expectancy declines and screening benefits tend to wane. Many conditions detected by routine screenings, such as prostate cancer or cervical cancer, typically take a while to cause trouble. A person in their 80s is more likely to die from another fatal condition before cervical cancer or prostate cancer would affect their health. Additionally, certain diseases, such as cervical cancer, become less common with advancing age.
As a result, many screening tests are not recommended forever: at some point in your life, your doctor may tell you that you no longer need to repeat a screening test, even one you finally got used to having.
Know when screening tests usually end
Expert guidelines for many common screening tests include an “end age” when people can reasonably stop having the test. For example:
- Pap smear: age 65
- mammogram: age 75
- colonoscopy: age 75
- chest CT scan (recommended for people with a significant smoking history): age 80.
There are exceptions, of course. For example, if a colonoscopy found abnormalities in an otherwise healthy 72-year-old, repeat testing after age 75 may be recommended.
Many women have Pap smears after guidelines suggest stopping
Pap smears screen for cervical cancer. In 1996, new guidelines recommended that women who received Pap smears at appropriate intervals before age 65 could safely stop.
Yet many women continue to have this screening after turning 65, according to a recent study published in JAMA Internal Medicine that looked at data from 15 to 16 million women per year between 1999 and 2019. Their average age was 76, most (82%) were white, and all were enrolled in Medicare.
The study found:
- In 1999, nearly three million women over age 65 (almost 19% of the study population) had Pap smears. By 2019, the number had fallen to 1.3 million (8.5%), a reduction of more than half.
- Among women older than age 80, about 3% had Pap smears.
- In 2019, the estimated cost related to Pap smears in these older women was $83.5 million.
Possibly, some women in this study had good reasons to continue having Pap smears. Perhaps they weren’t adequately screened when they were younger. Perhaps they had previous Pap smear abnormalities. Maybe their doctors recommended they continue having Pap smears despite their advanced age. We don’t know, because this study didn’t collect that information. Still, it’s quite likely that many (or even most) of these Pap smears represent overscreening: routine testing with little chance of benefit.
Why does overscreening matter?
Overscreening may cause
- discomfort that may be tolerable when there’s an expectation of benefit, but less acceptable when the test is unnecessary
- anxiety while awaiting the results of the test
- false-positive results that lead to additional testing and unnecessary treatment
- complications of testing, such as infection or bleeding after a Pap smear, or perforation or bleeding after a colonoscopy. (Fortunately, complications are rare.)
- unnecessary costs, including medical appointments and lab fees, time wasted, and taking health providers away from more valuable care.
The bottom line
Screening tests are typically performed for people without symptoms, signs, or a high suspicion of disease. In many cases, they’re looking for a condition that is probably not there. For most screening tests, we have guidelines developed by experts and backed by data suggesting when to start — and when to stop — screening.
But guidelines are only general recommendations, and individual preferences matter. If foregoing a screening test will cause you excessive anxiety, or if having a test will provide significant peace of mind, it may be reasonable to have a test even after the recommended end age. Be sure you understand potential downsides, such as additional tests and complications.
So, never hesitate to ask your doctor when your next screening tests are due — but don’t forget to also ask if they are no longer worth having.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD